
The Internal Medicine Residency at Baylor College of Medicine is committed to training the best physicians in the country. At the core of our curriculum is rigorous clinical training at our diverse hospitals and clinics, with increased clinical responsibility, leadership, and teaching over the years:
- PGY-1 Year: To build a strong foundation in internal medicine, interns spend approximately one-third of the year on general medicine wards teams. They also start exploring subspecialty interests with elective and critical care rotations, while building continuity clinic panels in primary care clinic.
- PGY-2 Year: Residents solidify skills in diagnosis, treatment, teaching, and care coordination on inpatient general medicine rotations (3 blocks). They also spend much of the year on inpatient and outpatient electives, in addition to continuity clinic, critical care, and (if requested) research rotations.
- PGY-3 Year: Senior residents consolidate patient care and teaching skills on inpatient medicine (3 blocks), ICU teams (2 blocks), and general medicine consults (1 block). They also continue to enjoy flexible blocks for subspecialty rotations, continuity clinic, and fellowship / job applications, finishing the year well-prepared for the next step in their careers.
Dedicated Tracks
For more rotation details, visit our dedicated track pages:
Didactics
In addition to the clinical training that takes place on general medicine and subspecialty inpatient and outpatient rotations, our program offers the following additional curricular elements:
- Resident-led morning report daily at each hospital – a fun, chief resident-facilitated session to practice clinical reasoning, socialize, and learn
- Noon conference sessions with high-yield teaching from faculty and chief residents once per week during protected learning time to cover our year-long curriculum
- Department of Medicine Grand Rounds weekly
- Wednesday School (academic day that includes ambulatory didactics, QI projects, High Value Care seminars, journal clubs, and resident-as-teacher workshops plus simulation sessions and procedure training) every other block
Mentorship
Each resident works on-on-one with a dedicated faculty advisor from the program leadership group or core educational faculty. Residents meet at least twice per year with advisors to review milestone-based evaluations, discuss career planning, and develop goals. Faculty advisors link residents with other mentors, including those in the trainees future career specialty. Visit our Fellowship and Careers page for more details on post-residency planning.
Innovative Educational Programs
The Internal Medicine Residency at BCM is known for its educational innovations, with many initiatives having been shared across the country via publications and national presentations & workshops. Our innovations include the following:•

Distinguished Educator Pathway: all residents interested teaching may participate in the Academy of Resident Educator curriculum and earn a certificate of distinction in medical education by the end of residency training.
Intern Bootcamp: annual day-long event during intern orientation in which PGY1s discuss common clinical scenarios one-on-one with a resident or faculty facilitator, practice safe patient handoffs, and review core skills such as calling consults, writing notes, and developing life-long learning habits during residency.

Longitudinal Point-of-Care Ultrasound (POCUS) Curriculum: year-long course that uses independent study, faculty-led didactics, and small group skills practice sessions to teach internal medicine-focused POCUS skills.
Wednesday School: protected academic half-day scheduled for each resident roughly every two months with a varied curriculum including clinical didactics, resident-as-teacher workshops, clinical reasoning sessions, reflection and self-care skills, and more.
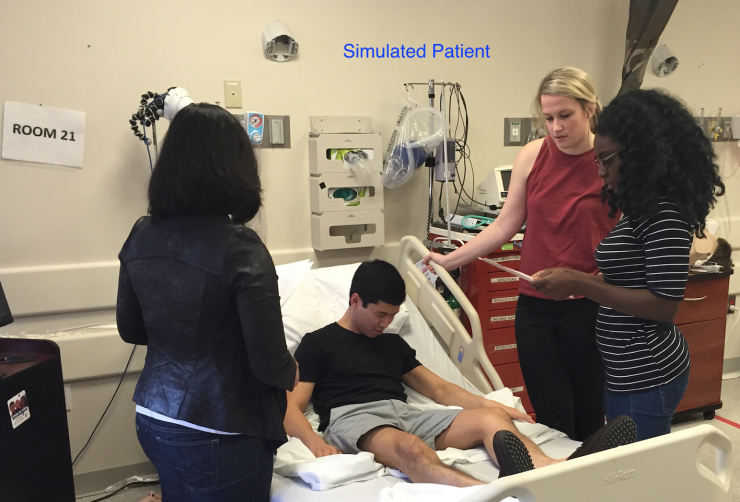
Clinical Simulation & Procedure: at the VA hospital simulation center, residents spend Wednesday School afternoons participating in rapid-response simulation scenarios and practicing procedure and ultrasound skills.
Upper Level Boot Camp: annual half-day of workshops that take place during Wednesday School for end-of-year PGY1s to prepare them for clinical leadership and team management roles as an upper level resident.
Cardiology Boot Camp: In collaboration with the Texas Heart Institute, BCM cardiology faculty & fellows lead this annual day-long workshop to teach interested residents important cardiology topics, such as Hemodynamics 101 or Intro to the Cath Lab.
Quality Improvement and Patient Safety Curriculum
Baylor College of Medicine Internal Medicine Residency Program places great emphasis on quality improvement and patient safety training, exceeding the requirements set forth by ACGME. The Internal Medicine Program hosts a comprehensive Quality Improvement (QI) curriculum, which includes a longitudinal course for PGY-2 residents based on the IHI Model for Improvement and Lean principles. PGY2 and PGY3 residents lead educational conferences on high-value care and patient safety. All residents participate in a QI project at our teaching hospitals. These award-winning resident projects have been presented at local, regional, and national level. Additionally, residents attend hospital committees that focus on systems-based practices including, Patient Safety, Quality Review, and Patient Flow. Residents may also choose to do a QI project as part of a month-long research elective.
For residents interested in pursuing quality improvement as a career, Baylor College of Medicine offers positions for Chief Residents in Quality and Patient Safety (CRQS) at the Michael E. DeBakey VA Medical Center.








