Researchers engineer better way to target leukemia cells
Acute Lymphoblastic Leukemia (ALL) is the most common childhood cancer. While most children respond well to chemotherapy, some experience resistant or relapsed disease. Building on an immunotherapy treatment called CAR T cell therapy, researchers at Baylor College of Medicine, working with colleagues from multiple institutions, were able to engineer a new fighter T cell that more effectively targeted leukemia cells in preclinical studies.
“Chimeric antigen receptor (CAR) T cell therapy, a form of immunotherapy, was developed to help children for whom chemotherapy was not enough,” said Dr. Nabil Ahmed, associate professor of pediatrics, section of hematology-oncology at Baylor College of Medicine and Texas Children’s Hospital. He is the senior author of the findings published by Dr. Kristen Fousek and colleagues in the journal Leukemia.
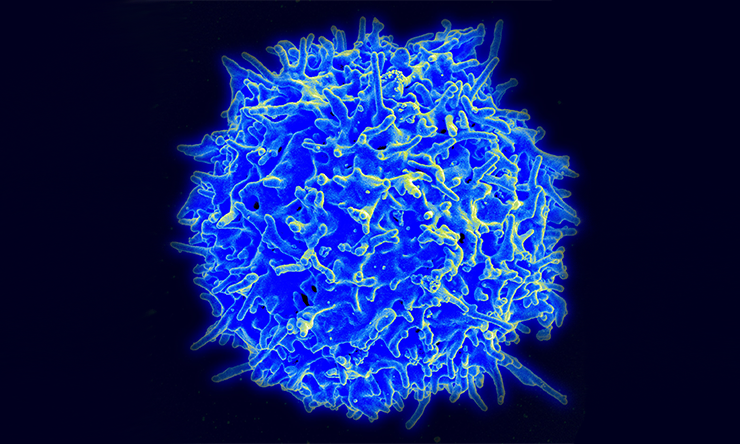
CAR T cell therapy uses a patient’s T cells, a type of immune cell that is usually involved in fighting cancer. Several research groups have genetically engineered patient’s T cells to express a CAR molecule to recognize CD19, a protein (antigen) found on leukemia cells. When these CAR T cells are introduced back into the patient, they can attack the cancer more effectively. Although initial treatment using CAR T cells offered impressive initial results, nearly half of the patients who received the therapy later relapsed because the cancer adapted to the attack by not producing the target protein CD19 anymore. As a result of this adaptation, the cancer became invisible to the engineered T cells.
Looking to improve this promising immunotherapy, Ahmed collaborated with Dr. Hisham Abdel-Azim, an investigator in the Saban Research Institute of Children’s Hospital Los Angeles and co-corresponding author, to study the pattern of target change before and after treatment with CD19 CAR T cells. Accordingly, Fousek, then a graduate student in Ahmed’s laboratory at the Center for Cell and Gene Therapy, engineered a T cell that targets not only CD19, but also two other proteins found on leukemia cells, CD20 and CD22.
“It’s like using a trident to attack the cancer instead of a spear,” Ahmed said. The team used this three-pronged weapon against leukemia cells in preclinical studies and developed new methods to monitor how well it worked.
The new CAR T cells, named TriCAR T cells, targeting CD19/20/22 were significantly more effective than T cells that target CD19 alone. When the leukemia cells stopped producing CD19 and were no longer visible to CD19 CAR T cells, TriCAR T cells were still effective.
“TriCAR T cells bind to more cancer cells and these connections are much stronger,” said Abdel-Azim. “We studied the behavior of individual TriCAR T cells in the laboratory of Dr. Varadarajan at the University of Houston; the new TriCAR T cells are more effective serial killers of leukemia,” Ahmed said.
Although a clinical trial will be needed before the new TriCAR T cell therapy could be used on patients, the early lab results suggest a path that could be significantly more effective in battling resistant leukemia.
See the publication to find the complete list of authors, their affiliations and sources of support for this project.







 Credit
Credit