Novel biomarker and potential improved therapy for MS and related disorders
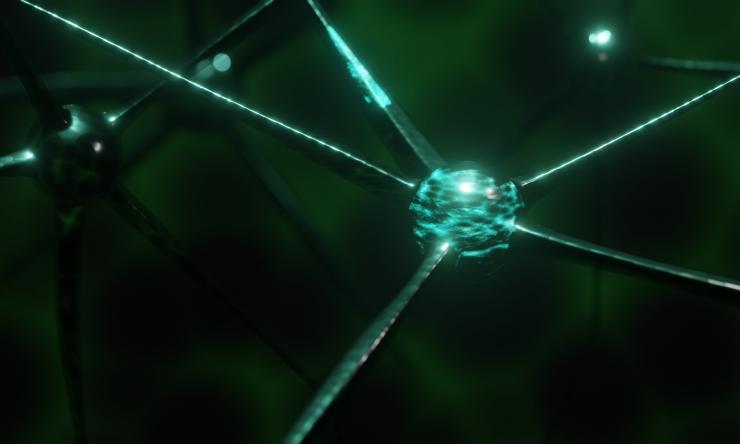
Degeneration of myelin, an insulating sheath required for rapid communication between nerve cells, is a notable hallmark of multiple sclerosis (MS) and related neurodegenerative disorders such as Alzheimer’s disease or Huntington’s disease. However, little is known about the precise molecular steps by which myelin degeneration leads to the loss of neurons and glia, the two major types of brain cells.
A team led by researchers at Baylor College of Medicine and the Jan and Dan Duncan Neurological Research Institute (Duncan NRI) at Texas Children’s Hospital report in the journal Cell Metabolism that myelin breakdown results in an accumulation of very long-chain fatty acids (VLCFA) and their intermediates, which triggers an autoimmune response that damages brain cells. Furthermore, reducing the levels of VLCFA using approved drugs bezafibrate and fingolimod had a synergistic beneficial effect on MS in an animal model, suggesting a potential more effective treatment for MS patients.
VLFCAs are a rare group of fatty acids or fats that comprise only a tiny fraction of the total fatty acids in the body. However, myelin sheaths that surround the nerve membranes are a rich source of VLCFAs when compared to other cellular membranes; therefore, during myelin degradation or aging, nerve cells are exposed to higher levels of VLCFA than normal.
Dr. Hyunglok Chung, a former postdoctoral fellow in Dr. Hugo Bellen’s lab who also is the first and co-corresponding author of this study, had previously reported that excess VLCFA is harmful to nerve cells in fruit flies. In the first part of this study, Chung and his colleagues show, also in fruit flies, that accumulation of S1P, a key product of VLCFA degradation, causes inflammation in nerve cells and potentially damages them.
The team then collaborated with co-corresponding author Dr. Hyun Kyoung Lee, associate professor of pediatrics – neurology at Baylor and investigator at the Duncan NRI, to explore the role of S1P in MS progression in a mouse model.
Co-first author Dr. Qi Ye, a postdoctoral associate in the Lee lab, found that pre-symptomatic treatment of these mice with bezafibrate, a lipid-lowering drug that inhibits the synthesis of VLCFA, slowed the progression of this debilitating disorder by reducing myelin loss, neuronal damage and infiltration of immune cells into the brain.
Qi next tested the potential therapeutic effect of lowering VLCFA and S1P on MS. “When we administered bezafibrate along with fingolimod at the onset of symptoms, we saw a synergistic improvement in paralysis and motor performance, and in myelin and neuronal loss. The combined effects of these drugs were significantly better than the effect of either drug alone in every parameter we tested, suggesting that a combined therapy could be more effective and offer better outcomes for MS patients,” Chung said.
“We are very excited by the potential clinical implications of this study not just in the treatment of MS but also for other neurodegenerative conditions that are associated with myelin loss, disruptions in lipid metabolism and neuroinflammation,” said Bellen, Distinguished Service Professor in molecular and human genetics at Baylor and the Duncan NRI. He also is a co-corresponding author of this study.
Others involved in the study were Ye-Jin Park, Zhongyuan Zuo, Jung-Wan Mok, Oguz Kanca, Sudhir Gopal Tattikota, Shenzhao Lu, Nobert Perrimon and Hyun Kyoung Lee. Their institutional affiliations can be found here. The study was funded by the National Institutes of Health, the Jan and Dan Duncan Neurological Institute at Texas Children’s Hospital, BCM IDDRC, Warren Alpert Foundation and others.
Read more details about this study here.