New insight into breast cancer resistance to hormone therapy
An international team of researchers led by scientists at Baylor College of Medicine has new insights into the function of neurofibromin, a tumor suppressor produced by the NF1 gene. It is well known that neurofibromin keeps cancer growth in check by repressing the activity of a cancer driver called Ras. The new research reveals a previously unknown function of neurofibromin — directly repressing gene expression controlled by the estrogen receptor-α (ER). Thus, when neurofibromin is lost, Ras and ER functions are both activated, causing treatment resistance and metastasis for ER+ breast cancer.
These findings, appearing in Cancer Cell, suggest that a therapeutic approach must combine two different drugs, a SERD (e.g., fulvestrant) to degrade ER and a MEK inhibitor (e.g., selumetinib or binimetinib) to inhibit Ras downstream signaling, in order to effectively treat neurofibromin-depleted ER+ breast cancer. When this combination therapy was tested in animal models, the result was tumor regression. The next step is to begin clinical trials of the effectiveness of this therapeutic approach in patients.
Neurofibromin loss drives tamoxifen and aromatase inhibitor resistance
This team first studied the importance of neurofibromin loss in a study they published in 2018 (Nature Communications PMC6123466) in which tumor DNA was sequenced to seek mutations that can promote resistance to tamoxifen, which is commonly used to prevent relapses from ER+ breast cancer.
“When we examined the mutational patterns in NF1, we observed that poor patient outcome only occurred when neurofibromin was lost, not through mutations that selectively affect Ras regulation. This suggested to us that neurofibromin may have more than one function,” said Dr. Eric C. Chang, one of two senior authors on the paper, an associate professor in the Department of Molecular and Cellular Biology and a member in the Dan L Duncan Comprehensive Cancer Center’s Lester and Sue Smith Breast Center.
This thought triggered studies, spearheaded by Dr. Zeyi Zheng in Chang’s lab, into the function of neurofibromin in ER+ breast cancer cells. One of his early experiments showed that when expression of NF1 is inhibited (to mimic neurofibromin loss in tumors), the resulting ER+ breast cancer cells were instead stimulated by tamoxifen and, not as usual, inhibited. Furthermore, these neurofibromin-depleted cells became sensitive to a very low concentration of estradiol, a form of estrogen.
“The clinical relevance of these findings was immediately apparent because it suggested that tamoxifen or aromatase inhibitors, which lower estrogen levels available to the cancer cells, would be the wrong choice for treatment when neurofibromin is lost by the tumor,” said co-senior author Dr. Matthew Ellis, professor and director of the Lester and Sue Smith Breast Center and a McNair Scholar at Baylor.
A key breakthrough: physically linking neurofibromin to ER
Follow-up gene expression studies all strongly suggest that neurofibromin behaves like a classic ER co-repressor.
“A co-repressor must bind ER directly, but the group hesitated to conduct such an experiment without more evidence because it is not trivial to do so,” Chang said.
A breakthrough came when Dr. Charles Foulds, a co-author on the paper and assistant professor at the Center for Precision Environmental Health at Baylor, searched the “Epicome,” a massive proteomic database created by Dr. Anna Malovannaya and Dr. Jun Qin at Baylor, as part of an effort by Dr. Bert O’Malley, chancellor and professor of molecular and cellular biology at Baylor, to comprehensively document all the proteins associated with ER. Foulds found neurofibromin in the database, which encouraged the team to ultimately demonstrate that ER and neurofibromin interact directly. However, to seriously consider NF1 as an ER co-repressor, there was still another missing piece of the puzzle.
“One day Charles casually asked me whether neurofibromin has a region rich in the amino acids leucine and isoleucine, because co-repressors use these motifs to bind ER, and it dawned on me that neurofibromin indeed does,” Chang said. “In fact, neurofibromin has two such motifs that mediate ER binding in a cooperative manner. These motifs are frequently mutated in cancers but are not required for Ras regulation.”
Approaches to treat neurofibromin-deficient ER+ breast cancer
Since tamoxifen or aromatase inhibitors were found to be ineffective for neurofibromin-deficent ER+ breast cancer tumors, preclinical models were used to show that the ER-degrading drug fulvestrant was still effective. However, fulvestrant only temporarily inhibited tumor growth because secondary Ras-dependent fulvestrant resistance was induced by neurofibromin-loss. This Ras-dependent growth phase could be inhibited with the addition of a MEK inhibitor, which shuts off a key signaling pathway downstream of Ras.
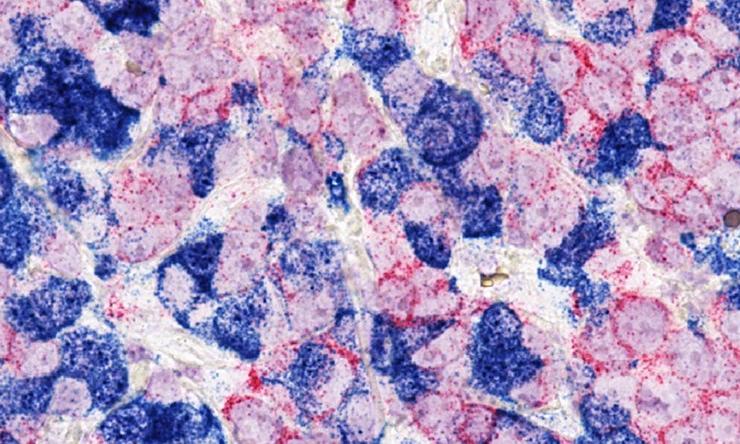
The team validated this combination treatment strategy using a patient-derived xenograft (PDX) mouse model which can maintain the genomics and drug response of the original human tumor from which is was derived (Cell Reports 2013 PMC3881975). In this case, this PDX was derived from a patient who failed several lines of endocrine therapy and already developed fulvestrant resistance.
“The results of the combination therapy were encouraging — the tumor shrunk to almost undetectable levels,” Chang said. “Our next goal is to test this combination therapy in clinical trials in order to determine its therapeutic potential in the clinic.”
“Neurofibromin loss is present in at least 10% of metastatic ER+ tumors. As a result of these new data, we are now working on a clinical trial that combines a MEK inhibitor, with fulvestrant,” said Ellis, Susan G. Komen scholar and associate director of Precision Medicine at the Dan L Duncan Comprehensive Cancer Center at Baylor. “Interestingly, MEK inhibitors are also being used to control peripheral nerve tumors in patients with neurofibromatosis, where a damaged NF1 gene is inherited. Our findings contribute to an understanding of why female neurofibromatosis patients also have a much higher incidence of breast cancer.”
Other contributors to this work include Meenakshi Anurag, Jonathan T. Lei, Jin Cao, Purba Singh, Jianheng Peng, Hilda Kennedy, Nhu-Chau Nguyen, Yue Chen, Philip Lavere, Jing Li, Xin-Hui Du, Burcu Cakar, Wei Song, Beom-Jun Kim, Jiejun Shi, Sinem Seker, Doug W. Chan, Guo-Qiang Zhao, Xi Chen, Kimberly C. Banks, Richard B. Lanman, Maryam Nemati Shafaee, Xiang H.-F. Zhang, Suhas Vasaikar, Bing Zhang, Susan G. Hilsenbeck, Wei Li and Charles E. Foulds. The authors are affiliated with one or more of the following institutions: Baylor College of Medicine, Chongqing Medical University, Adrienne Helis Malvin Medical Research Foundation, Zhengzhou University and Guardant Health.
See the publication for a complete list of the sources of support for this work.







 Credit
Credit