Long-term survival following CAR T cell therapy to treat neuroblastoma
An 18-year survivor of neuroblastoma, a solid childhood tumor that develops in immature nerve cells, is believed to represent the longest reported remission to date in a patient treated with chimeric antigen receptor (CAR) T cell therapy. The findings, published in Nature Medicine, describe several long-term survivors in a follow-up from a phase 1 clinical trial for a genetically engineered CAR T cell therapy developed at the Center for Cell and Gene Therapy at Baylor College of Medicine, Texas Children’s Hospital and Houston Methodist Hospital.
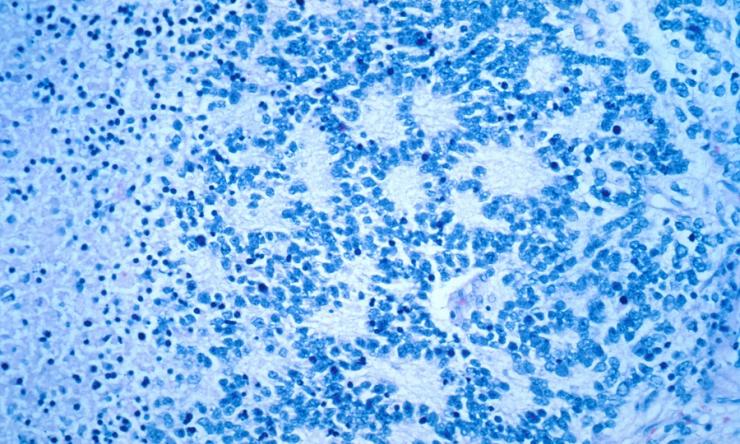
The trial (NCT00085930), which enrolled patients from 2004 to 2009 at Texas Children’s Cancer Center, was the first study opened at the Center for Cell and Gene Therapy. Nineteen children with relapsed or refractory neuroblastoma were treated with CAR T cells engineered to target GD2, an antigen highly expressed on the surface of neuroblastoma cells. Out of 11 patients with active disease at the time of treatment, two had sustained complete responses, one of those for more than 18 years. Of eight patients with no evidence of active disease at the time of treatment, five were disease free at their last follow-up between 10-15 years after infusion.
“Our findings suggest that even with this early study some patients can have long-lasting benefit,” said corresponding author Dr. Helen Heslop, director of the Center for Cell and Gene Therapy, deputy director of the Dan L Duncan Comprehensive Cancer Center and Dan L Duncan Chair at Baylor.
Investigators detected low levels of CAR T cells persisting in patients during the follow-up observation period, with higher persistence detected in long-term survivors. The first-generation CAR T therapy used in this trial did not include co-stimulatory molecules, which are used in current CAR T therapies to improve effectiveness.
“We’re encouraged that it’s not just patients with certain malignancies of blood cells who can have sustained responses to CAR T cells, but also some patients with advanced solid tumors who can still be disease free almost two decades later, with normal quality of life,” said co-author Dr. Malcom Brenner, professor and founding director of the Center for Cell and Gene Therapy and Fayez Sarofim Chair at Baylor. “In the future, we hope to extend this success to a higher percentage of patients in more types of cancer.”
“This was a landmark trial to demonstrate the feasibility and the long-term outcomes of cell therapy to treat solid tumors, even using the first-generation CAR T cell therapy,” said first author Che-Hsing Li, graduate student in pediatrics – oncology at Baylor.
Other authors who contributed to this work include Sandhya Sharma, Andras A. Heczey, Mae L. Woods, David H. M. Steffin, Chrystal U. Louis, Bambi J. Grilley, Sachin G. Thakkar, Mengfen Us, Tao Wang and Cliona M. Rooney. They are affiliated with the Center for Cell and Gene Therapy, Center for Advanced Innate Cell Therapy and the Dan L Duncan Comprehensive Cancer Center at Baylor College of Medicine.
See the publication for a complete list of funding for this work.