CAR-NKT cell therapy shows promising results against neuroblastoma in phase 1 clinical trial
Researchers at Baylor College of Medicine/Texas Children’s Cancer Center and collaborating institutions report interim results from a first-in-human phase 1 clinical trial evaluating the safety, antitumor activity and immunological characteristics of a genetically engineered natural killer T (NKT) cell immunotherapy for neuroblastoma, a childhood tumor that most commonly arises in the adrenal gland. The study published in Nature Medicine shows the treatment was well tolerated, and researchers observed early evidence of strong antitumor activity.
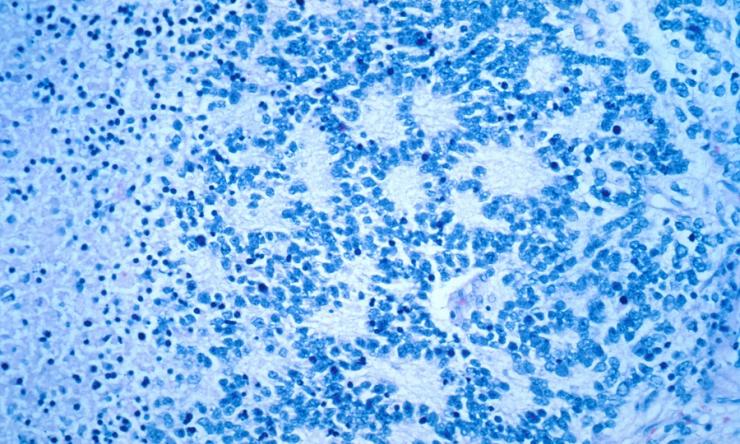
NKT cells were modified to express a GD2-specific chimeric antigen receptor (GD2 CAR), which enables the immune cells to target a molecule found on the surface of neuroblastoma cells, and interleukin-15 (IL-15), a natural protein that supports NKT cell survival. In a previous Nature Medicine publication, the authors reported interim results from the first three children enrolled on this trial.
In the new article, investigators describe the results obtained in 12 patients with stage 4 relapsed neuroblastoma that was resistant to other therapies. They found that the therapy was safe for all 12 patients on four dose levels; there were no reported no dose-limiting toxicities. Three patients showed an objective response to treatment, including one complete response and two partial responses. Two other patients also showed evidence of antitumor activity such as clearance of bone marrow involvement or reduction of metastatic tumor burden not reaching partial response criteria.
“We are encouraged by the evidence of antitumor activity that has been observed in several patients, particularly since this trial is still in the dose escalation phase,” said Dr. Andras Heczey, co-corresponding author and associate professor of pediatrics – hematology and oncology at Baylor. He also is a member of the Center for Advanced Innate Cell Therapy at Texas Children’s Cancer Center, the Center for Cell and Gene Therapy at Baylor and Texas Children’s and the Dan L Duncan Comprehensive Cancer Center at Baylor.
Previous studies from the team have shown that NKT cells can localize to tumor sites in pre-clinical models. This trial has validated those observations in humans. Additionally, researchers found a correlation between higher antitumor activity and in vivo proliferation of infused CAR-NKT cells.
“We cannot always predict the extent of NKT cell expansion in vivo after infusion,” said Dr. Leonid Metelitsa, co-corresponding author and professor of pediatrics – hematology and oncology at Baylor. “In this study, we found the CD62L biomarker expressed on the infused NKT cells, which we identified in our preclinical work, is predictive of both higher NKT cell in vivo expansion and antitumor activity in patients.” Metelitsa is also director of the Center for Advanced Innate Cell Therapy at Texas Children’s Cancer Center and a member of the Center for Cell and Gene Therapy at Baylor and Texas Children’s and the Dan L Duncan Comprehensive Cancer Center at Baylor.
Another important finding revealed a regulatory gene in NKT cells that may impact the efficacy of treatment. Leveraging the multiomic platform of key collaborator Immunai, Inc., Baylor researchers found that upregulation of the BTG anti-proliferation factor 1 (BTG1) gene in infused CAR NKT cells is indicative of cell exhaustion and restricts CAR NKT cell functional activity. Conversely, engineered reduction of BTG1 expression in CAR NKT cells enhanced their therapeutic activity against neuroblastoma in a mouse model.
“This study provides promising initial evidence of antitumor activity of GD2 CAR NKT cells against neuroblastoma. This inspires hope that novel immunotherapeutic strategies, such as the one studied in this trial, will ultimately improve the outcomes for children with neuroblastoma,” Metelitsa said.
Based on the safety profile and promising evidence of antitumor activity, this trial has been expanded to include two higher dose levels for the GD2 CAR NKT cells. Following completions of these additional cohorts, a phase 2 trial to assess the antitumor activity of this novel immunotherapeutic is planned.
Other contributors to this work include Xin Xu, Amy N. Courtney, Gengwen Tian, Gabriel A. Barragan, Linjie Guo, Claudia Martinez Amador, Nisha Ghatwai, Purva Rathi, Michael S. Wood, Yanchuan Li, Chunchao Zhang, Thorsten Demberg, Erica J. Di Pierro, Andrew C. Sher, Huimin Zhang, Birju Mehta, Sachin G. Thakkar, Bambi Grilley, Tao Wang, Brian D. Weiss, Antonino Montalbano, Meena Subramaniam, Chenling Xu, Chirag Sachar, Daniel K. Wells and Gianpietro Dotti. The authors are affiliated with the following institutions: Baylor College of Medicine, Texas Children’s Hospital, Cincinnati Children’s Hospital, Immunai, Inc., and University of North Carolina at Chapel Hill.
This work was supported by Alex’s Lemonade Stand Foundation for Childhood Cancer, St. Baldrick’s Foundation, the American Cancer Society and Athenex, Inc. For a full list of author affiliations and funding for this work, refer to the publication.