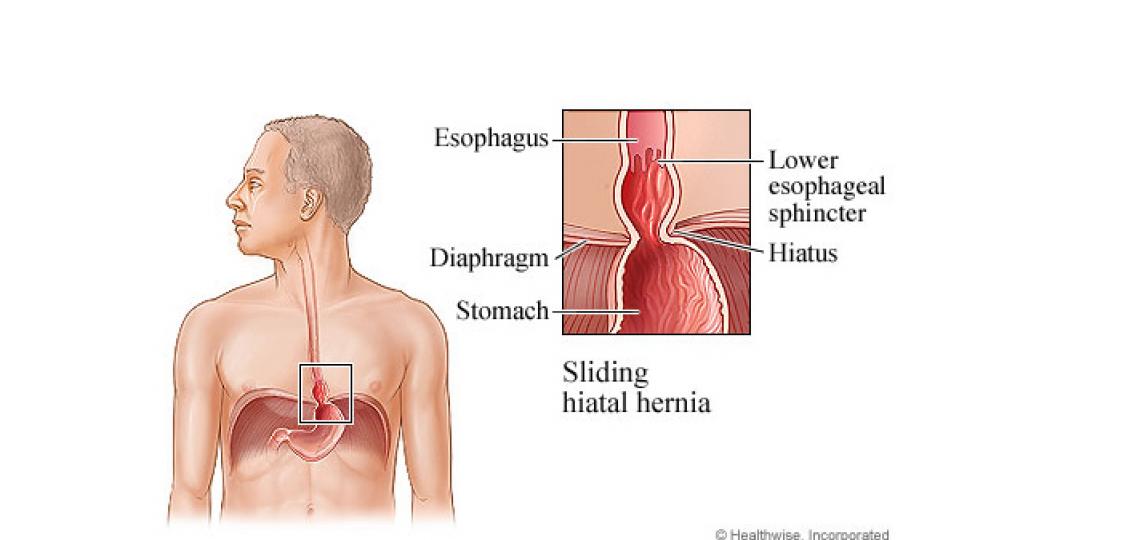
A hiatal hernia occurs when a small portion of the stomach pushes upward through the diaphragm, a sheetlike muscle that separates the lungs from the abdomen. Usually this doesn't cause any symptoms, but it increases the risk of stomach acid backing up into the esophagus (reflux), which can lead to heartburn.
Normally the entire stomach sits below the diaphragm. The esophagus passes through an opening in the diaphragm called the hiatus before it enters the stomach. Weakened tissues within and around the hiatus allow a hiatal hernia to develop.
A hiatal hernia that is not causing symptoms does not usually need any treatment. Treatment for a hiatal hernia that causes heartburn is the same as for gastroesophageal reflux disease (GERD). This may include home treatment with lifestyle changes; nonprescription antacids, acid reducers, or acid blockers; prescription medicines; or, in severe cases, surgery.
How is a hiatal hernia diagnosed?
A hiatal hernia often is diagnosed when you see your doctor or have tests for another health problem, especially if it is small or does not cause you symptoms.
If you have symptoms, your doctor will ask you questions about them. If your symptoms happen often and are severe, you may have gastroesophageal reflux disease (GERD). If this is the case, your doctor may do more tests or give you medicine to treat GERD.
Some patients may undergo an esophagram or CT scan to diagnose a hiatal hernia. Your doctor will discuss any tests they recommend and the results with you in order to formulate a plan of care that is best for you.
What are the symptoms of a hiatal hernia?
Most people who have a hiatal hernia have no symptoms.
One symptom you may have is heartburn, which is an uncomfortable feeling of burning, warmth, or pain behind the breastbone. It is common to have heartburn at night when you are trying to sleep.
If you often have symptoms or they are severe, you may have gastroesophageal reflux disease (GERD). A hiatal hernia can lead to GERD, and people often have both conditions at the same time.
If you have pain behind your breastbone, it is important to make sure it is not caused by a problem with your heart. The burning sensation caused by GERD usually occurs after you eat. Pain from the heart usually feels like pressure, heaviness, weight, tightness, squeezing, discomfort, or a dull ache. It occurs most often after you are active.
Some patients have a chronic cough, wake up with an acidic taste in their mouth, feeling full quickly after eating, or regurgitation of food. Abdominal pain after eating can have a variety of causes, and it is important to discuss with your doctor so you can get the appropriate diagnosis and treatment.
How is a hiatal hernia treated?
If you have no symptoms, you don't need treatment.
If you have mild symptoms, your doctor may suggest lifestyle changes and nonprescription medicines. Here are some things to try:
- Change your eating habits. Some people have certain foods that trigger their reflux. Chocolate, mint and alcohol can make GERD worse. They relax the valve between the esophagus and the stomach. Spicy foods, foods that have a lot of acid (like tomatoes and oranges) and coffee can make GERD symptoms worse in some people. If your symptoms are worse after you eat a certain food, you may want to stop eating that food to see if your symptoms get better.
- Eat several small meals a day instead of two or three large meals.
- Sit upright for two to three hours after you eat before you lie down. Late-night snacks can worsen reflux symptoms
- Do not smoke or chew tobacco. Talk to your doctor if you need help quitting.
- Raise the head of your bed 6 in. (15 cm) to 8 in. (20 cm) by putting the frame on blocks or placing a foam wedge under the head of your mattress if you get heartburn at night.
- Do not wear tight clothing around your midsection.
- Lose weight if you need to. Losing just five to ten pounds can help reduce reflux symptoms.
If you have symptoms that have a significant impact on your lifestyle or if you have severe symptoms, you may have GERD. Lifestyle changes may help, and your doctor may prescribe medicines like Proton Pump Inhibitors or PPIs. In severe cases, surgery can be used to pull the hernia back into the belly.
Hiatal Hernia Surgery
Depending on the size of your hernia, your surgeon will discuss with you the most appropriate approach to fix your hiatal hernia. Many patients are able to have their hernia repaired through minimally invasive surgery, also called laparoscopic or robotic laparoscopic surgery, which offers a faster, less painful recovery.
The goal of the surgery is to restore the normal anatomy of your organs, so your surgeon will work to bring down the stomach into your abdomen, below the diaphragm. Next, your surgeon will work to make the hole in your diaphragm (also known as the hiatus) small enough to prevent your stomach or abdominal organs from herniating into your chest. This is usually done by stitching your diaphragm to itself but sometimes requires a small piece of mesh.
Hiatal hernia surgery is often combined with other surgeries to address GERD symptoms, such as LINX or Fundoplication.
Recovery from Hiatal Hernia Surgery
Recovery from hiatal hernia surgery usually takes four to six weeks, but many patients feel better very quickly after surgery and can even return to work in one to two weeks. You can expect to spend one to two nights in the hospital after your surgery. You will be instructed to follow a liquid or soft foods diet for a few weeks to allow time for swelling to go down and for your stomach to heal. Your surgeon might instruct you to take crushed or liquid medications during your recovery. You should stay active after surgery – walking starts on day one after surgery. You should gradually increase your activity level back to your baseline. Your surgeon might instruct you to limit how much weight you lift, but a general rule during recovery is do not do anything that causes you pain.
If you have any questions or concerns about your recovery, you should speak with your surgeon as soon as possible to prevent complications.







 Credit
Credit