What is Pericarditis?
Pericarditis refers to swelling and irritation of the layers of sac-like tissue that is surrounding the heart. A small amount of fluid will ensure the layers stay separate and have no friction between them. Pericarditis can cause sharp chest pains that begin when the irritated or swollen layers begin to rub on each other. Pericarditis is typically mild and can be managed on its own or with simple treatment. If treatment is needed, it can include medication and rarely will include surgery.
Cause of Pericarditis
The root cause of pericarditis is sometimes hard to determine, or deemed to be unknown.
Possible causes of pericarditis are:
- Heart attack and/or heart surgery, which may trigger pericarditis or cause delayed pericarditis
- Infection from viral or respiratory agents
- Systemic inflammatory disorders such as rheumatoid arthritis and/or lupus
- Trauma suffered from a motor vehicle or other accident to your heart or chest
- Other health disorders, including but not limited to kidney failure, AIDS, tuberculosis, and cancer
- Medication
Symptoms
Pericarditis can cause chest pain, which is the most common of the symptoms. This will typically feel like sharp pains. Although, it may feel dull, achy, or pressure-like.
The pain may be felt behind the breastbone or left side of the chest. There is a possibility that it will spread or migrate to your left shoulder or neck region. You may notice an increase in the symptoms when you either cough, lie down, or attempt to take a deep breath, and will feel relief when you sit up or lean forward.
Additional symptoms can include:
- Shortness of breath while lying down
- Low-grade fever
- Heart palpitations
- Fatigue
- Cough
- Abdominal or leg swelling
Specific symptoms will be determined based off the type of pericarditis you have. It is grouped into four different categories, based on patterns and longevity of the symptoms.
Acute Pericarditis begins abruptly but doesn’t last longer than three to four weeks.
Recurrent Pericarditis can typically last for four to six weeks after an episode of acute pericarditis.
Incessant Pericarditis occurs for about four to six weeks but will last less than three months. The symptoms experienced during this category, are continuous.
Chronic Constrictive Pericarditis will develop slowly and last longer than a three-month time span.
Diagnosing Pericarditis
If you are experiencing sharp pains in your chest and on the back of your shoulders and experiencing difficulty breathing, these are two major indicators that you may have pericarditis. Your doctor will begin by listening to your heartbeat, seeing if they can hear a rubbing or creaking sound, which is caused by the rubbing of the inflamed pericardium.
Blood tests will be performed to check for any indication of a heart attack, inflammation, and/or infection. Additional tests used to diagnose pericarditis include:
Electrocardiogram (ECG): a quick test that records electrical signals in your heart.
Chest X-Rays can show changes in the size and shape of your heart and if there is any excess fluid.
Echocardiogram or sound waves used to create a picture of your heart and the surrounding lining.
Cardiac computerized tomography (CT) scan uses X-rays to create images of your heart and chest and may help to show thickening of the pericardial lining.
Cardiac magnetic resonance imaging (MRI) uses a magnetic field and radio waves to create cross-sectional images of the heart. MRI is an important test for chronic pericarditis which will help show if the lining is severely thickened and would benefit from resection. The MRI can also show the function of the heart and tell us if the chronic inflammation is obstructing normal blood flow.
Treatment
Treatment plans will depend on both the cause and the severity of your symptoms. Typically it is seen that mild cases may get better on their own without treatment.
Some cases may be treated with medication to reduce the inflammation and swelling. Some of these include:
- Pain relievers
- Colchicine
- Corticosteroids
Surgeries or alternative procedures
If there has been fluid that is building up around the heart, you may need to have it drained with a needle, small tube, or open surgery. The treatment plans include
Pericardiocentesis: the doctor will use a small catheter to remove the excess fluid from the pericardial cavity and this will stay in place for several days.
Pericardial window: The surgeon will make a small incision at the very bottom of the sternum to access the pericardial sac and drain any fluid. An alternative approach is to use a camera through the side of the chest. The pericardial window may be used ahead of pericardiocentesis or after recurrence of effusion after pericardiocentesis.
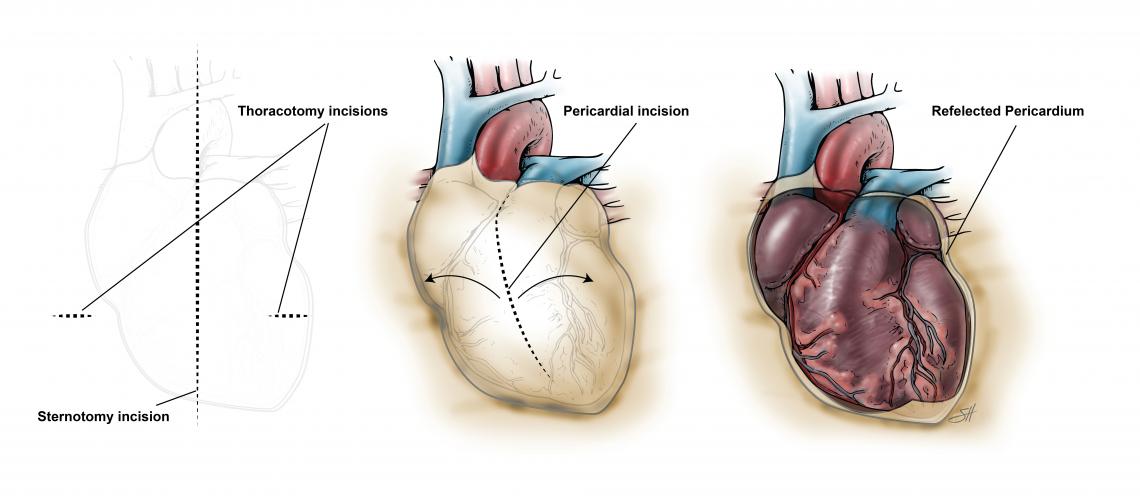
Pericardiectomy: this will remove the entire pericardium. This is typically reserved for cases of chronic pericarditis where the thickened sac is causing obstruction of normal heart function. In this procedure, the surgeon will remove as much of the pericardium as possible while avoiding injury to critical structures. These structures include the coronary arteries and the phrenic nerves that control diaphragm function. It is important to have this surgery done at a center that uses a multidisciplinary team skilled in the diagnosis and management of chronic pericarditis. In addition, this procedure may be performed through the front of the chest (sternotomy) or through the sides (thoracotomy) depending on the extent of the disease. Also, the surgery may or may not require the use of cardiopulmonary bypass to assist the heart. This is often the case when there is very extensive thickening that needs to be removed behind the heart.







 Credit
Credit