Inclusion body myositis, an inflammatory myopathy, has increasingly been recognized as the most common cause of muscle weakness diagnosed in older individuals. In addition, several patients with refractory polymyositis have, upon reevaluation of their diagnosis, been diagnosed with inclusion body myositis. The symptoms differ slightly from the other inflammatory myopathies in that the weakness seems to affect the distal and flexor muscles of the hands and quadriceps muscles more severely than other muscle groups.
Diagnosis
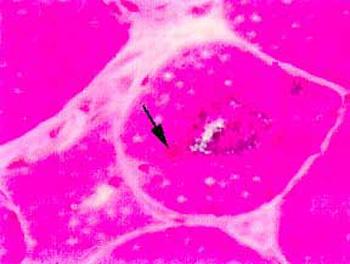
The diagnosis of inclusion body myositis is suspected in the presence of the history and examination compatible with a chronic acquired muscle disease. Once the diagnosis is suspected, the initial diagnostic steps include obtaining blood for CPK level and a muscle biopsy. The muscle biopsy of inclusion body myositis shows mild to moderate inflammation, atrophic denervated fibers, and most characteristically "rimmed vacuoles" as well as some muscle fibers with eosinophilic inclusions. Abnormal deposits of a substance called amyloid can be demonstrated upon histologic examination in and around the vacuoles and inclusions.
At present there is no effective treatment for inclusion body myositis. Several treatments using various immunosuppressants have not shown significant benefit, although there are anecdotal reports of certain patients responding to various immunosuppressive medications. Recent reports suggesting a beneficial effect of treatment with high doses of intravenous gamma globulin in a very small group of patients awaits confirmation.