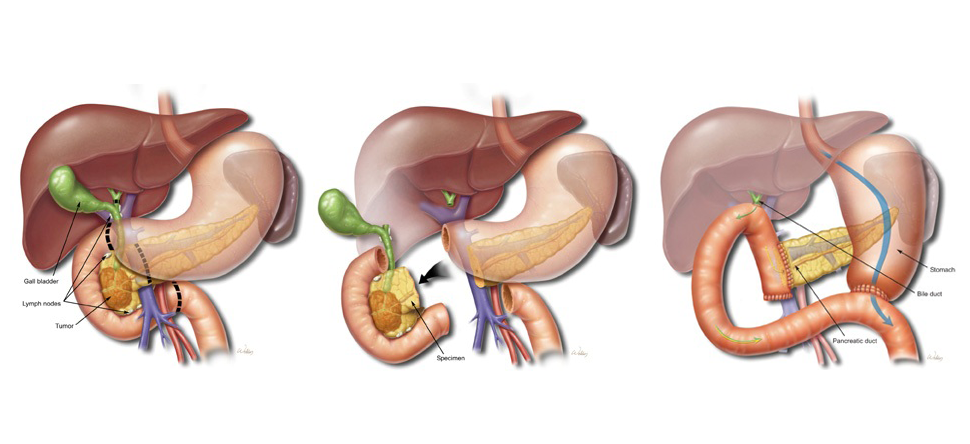
Also called a pancreaticoduodenectomy, the Whipple procedure is performed to address chronic pancreatitis and cancer of the pancreas, ampulla of Vater, duodenum, and the distal bile duct. It is a surgery in which the head of the pancreas, gallbladder, stomach and part of the small intestine, and the bile duct are removed. Enough of the pancreas is left to produce digestive juices and insulin.
In the beginning of the procedure, the surgeon will decide whether the tumor can be removed. The pancreas is examined by an open incision or by laparoscopic instruments. If the cancer has not spread to surrounding tissues, your surgeon will continue to perform the Whipple procedure.
The neck of the pancreas is divided in front of the portal vein. The duodenum is divided below the stomach, and farther downstream. The bile duct is divided just above the gallbladder. The pancreas, bile duct, and stomach have to be reconnected to the small intestine. This restores digestive function by re-establishing the flow of pancreatic juice from the pancreatic duct, bile from the bile duct, and food from the stomach. The specimen removed includes the head of the pancreas with the tumor and lymph nodes, a segment of duodenum, the bile duct, and the gallbladder. In some cases, the tumor has grown into the portal vein. In selected patients, a segment of the vein can be removed along with the tumor. The vein can be replaced using the internal jugular vein from the neck.
The next steps reconnect the intestinal tract. The stomach is connected to the small intestine, and the bile duct and remaining portion of the pancreas are reattached. Several tubes be implanted for postoperative care. To prevent tissue fluid from accumulating in the operated site, a temporary drain leading out of the body will be implanted.
What Happens on the Day of Surgery?
You will report to a preoperative nursing unit, where you will change into a hospital gown. A nurse will review your chart and confirm that all paperwork is in order. You will be taken to a pre-operative holding area, where an anesthesiologist will start an IV. Before any medications are administered, your surgeon will verify your name and the type of procedure you are having, and answer any further questions. You will then be taken to the operating room. After the appropriate form of anesthesia is administered, surgery will be performed.
What Type of Anesthesia Will Be Used?
You will have a pre-operative interview with an anesthesiologist, who will ask you questions regarding your medical history. A Whipple procedure is performed with general anesthesia, which will keep you asleep during surgery.
What Happens After the Surgery?
Once the surgery is completed, you will be taken to a post-operative or recovery unit where a nurse will monitor your recovery. It is important that your bandages be kept clean and dry. You will experience pain in your abdomen so your surgeon will give you a prescription for pain medication.
What Are the Risks Associated with a Whipple Procedure?
As with any surgery, there are risks such as bleeding, infection, or an adverse reaction to anesthesia. Biliary and pancreatic leaks may also occur. Because the pancreas will not function as effectively, postoperative diabetes and the occurrence of fatty stool may develop. This depends upon how much of the pancreas remains. Your surgeon will inform you of the risks prior to surgery.
What Should I Watch Out For?
Be sure to call your doctor if any of the following symptoms appear:
- Fever
- Worsening pain
- Redness or swelling around the incision
- The incision is warm to the touch
- Drainage from the incision
Will There Be Scars?
There will be a scar on your abdomen. Dr. Fisher closes the wound with subcutaneous suture, to assure the best possible cosmetic result.
When Can I Return to Work and Resume Normal Activities?
This varies from patient to patient. Patients experience pain and weakness after the Whipple procedure. Eating and finding the right foods will be difficult for the first few weeks. You may also experience nausea and constipation. Because of these difficulties, you will probably be unable to resume work and normal activities within the first month of recovery. After the first month, you will slowly begin to feel normal.
At The Elkins Pancreas Center, a team of doctors including surgical, medical, and radiation oncologists, gastroenterologists, radiologists, and pathologists will participate in your care. These doctors work together in a coordinated fashion to develop the best individualized treatment plan for you. Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, to kill the cells or to stop the cells from dividing. Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells.
If the pancreatic cancer has spread (or metastasized), or if the cancer grows back, palliative surgery and treatment might be recommended. The purpose of palliative treatment is to provide relief from the symptoms of the cancer. For more information, see Palliative Care.
Where To Go For Surgery

Our doctors perform surgery at Baylor St. Luke's Medical Center. If surgery is recommended, the nurse will give you instructions on where to report and when. She will also provide other instructions you will need to prepare for surgery. This may consist of consultations with cardiology and pulmonary physicians, and possible immunizations. Please do not hesitate to contact us if there are any questions about your preoperative instructions.







 Credit
Credit